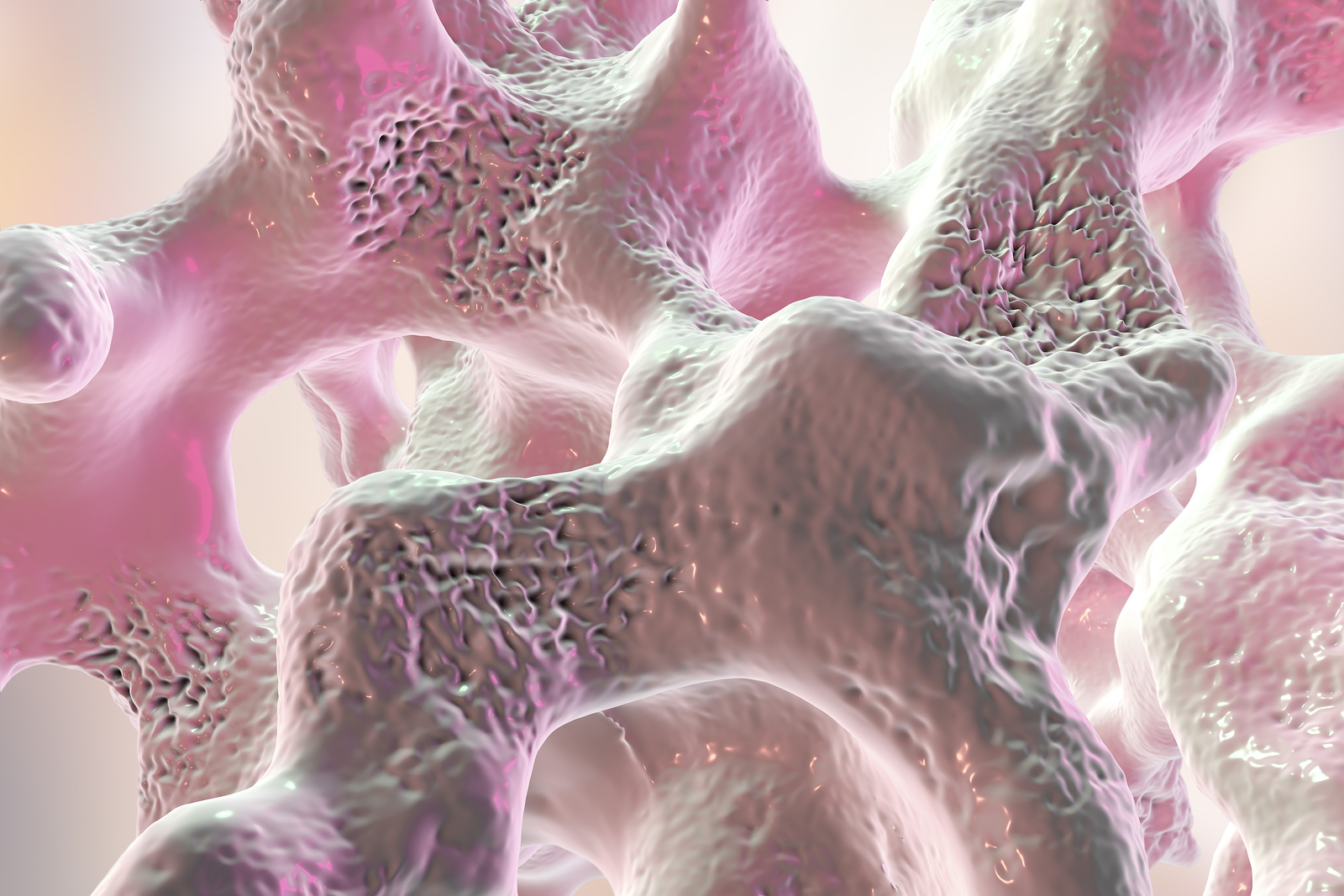
Bones are complicated living tissue, not ossified shells around marrow like soup bones you bring home from the butcher. Bones are 35% latticed protein—an infrastructure known as the collagen matrix—and 65% mineralized collagen, which gives the bone its strength.
Bone health depends on a give-and-take process, called remodeling. During this process, bone cells called osteoclasts travel through bone tissue retrieving old bone and leaving small, jagged spaces behind. This triggers their counterparts, called osteoblasts, to come in and fill these spaces and deposit new bone. About 5-10% of all our bone tissue is replaced—or turned over— in a year in this way. Osteoblasts cannot work properly without sufficient osteoclast activity, and new bone is stronger and—this is key—more flexible than old bone.
Healthy bones store about 99% of the body’s calcium; the rest is used throughout the body for other vital functions. Bones also house about 85% of the body’s phosphorus and about 50% of the body’s total sodium and magnesium.
Women with healthy bones still experience bone loss as they age. The bell curve looks something like this: During puberty, when our body and skeleton are growing, bone formation outpaces bone loss. By our early 30’s, most women (and men) have reached peak bone mass. By the late 30’s, bone resorption is slightly higher than formation (about .5-1%). After menopause this rate accelerates to 1-5% , on average, depending on a woman’s diet, exercise, body frame, drug intake, and overall health. Within five years after menopause, bone loss evens out again to a gradual and healthy decline of 1-1.5% per year. If you have osteoporosis, however, this rate of bone loss goes into hyper drive. Some women can lose up to 25% of their bone density in the ten years following menopause.